Senator John Fetterman’s courageous decision to seek treatment for major depression at Walter Reed National Military Medical Center in 2023 sparked a nationwide discourse on the significance of open discussions around mental health. This conversation has shed light on the intricate relationship between stroke recovery and mental well-being, emphasizing the importance of timely intervention and comprehensive care for individuals battling severe depression.
Understanding Clinical Depression
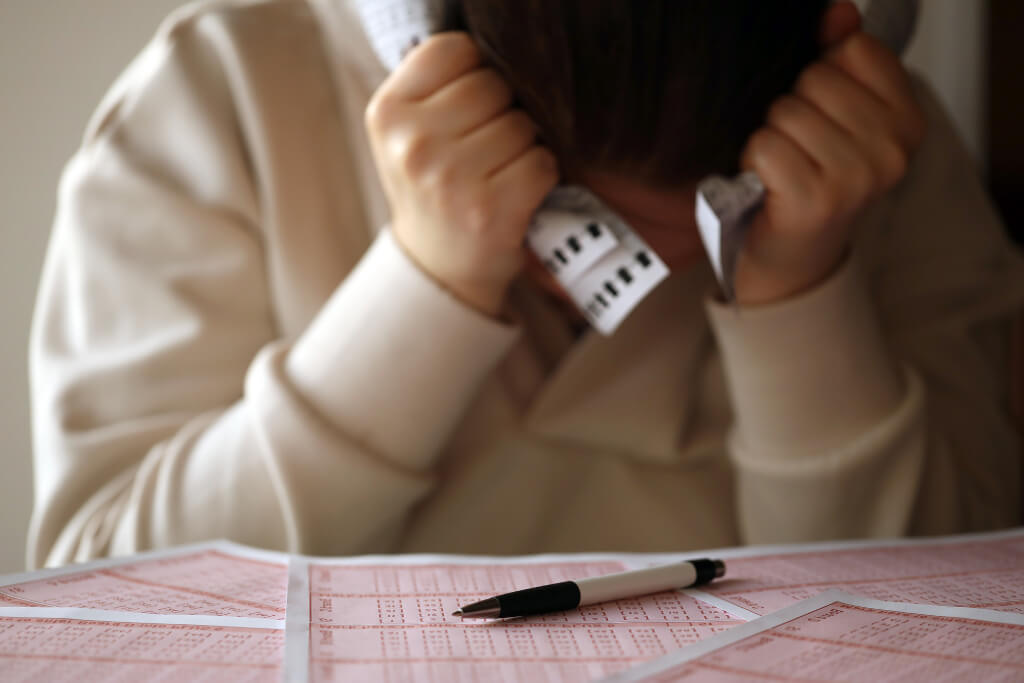
Characterized by a spectrum of emotional disturbances, clinical depression, or major depressive disorder, impacts approximately 20% of individuals at some point in their lives. The manifestation of this condition can vary, often leading to a profound loss of interest in previously enjoyed activities, disrupted sleep patterns, changes in appetite, persistent fatigue, irritability, and difficulties with concentration and decision-making. To warrant a clinical diagnosis, these symptoms must persist for a minimum of two weeks.
Various triggering factors such as bereavement, divorce, or job loss can precipitate depressive episodes. Moreover, underlying physical ailments like stroke or thyroid disease can exacerbate depressive symptoms, compounding the challenges of recovery and well-being. Left untreated, severe depression can result in a deterioration of overall health and a diminished quality of life.
Recognizing the Urgency of Intervention
When persistent shifts in mood endure and are coupled with suicidal thoughts, immediate action becomes imperative. Whether the result of a severe depressive episode or secondary to other underlying issues, the presence of suicidal ideation demands urgent attention. Suicidal ideation can manifest in passive forms, such as feelings of hopelessness, or take on an active and deliberate nature, involving specific plans for self-harm.
Understanding the warning signs and risk factors associated with suicide is critical. Feelings of hopelessness heightened anxiety, and a lack of purpose can exacerbate the vulnerability to suicidal tendencies, often accompanied by sleep disturbances and an increased inclination toward risky behaviors, including substance misuse. Withdrawal from social circles and a preoccupation with mortality further indicate the need for immediate intervention.
Exploring Inpatient Care for Depression
In cases where a more structured and intensive approach is necessary, inpatient mental health care can prove to be a vital resource. While individuals with a heightened risk of suicide benefit significantly from the supportive environment of inpatient care, those grappling with substance abuse, hallucinations, paranoia, or mania associated with bipolar disorder can also find solace in such a setting.
The primary goal of inpatient care facilities is to establish a secure and nurturing environment with continuous monitoring. Comprehensive assessments and medication management, if required, are integral components of the treatment process. Furthermore, individual and group psychotherapy, alongside expressive therapies like art and writing, contribute to the holistic healing process. Equipping patients with coping mechanisms and providing access to vital resources remain central objectives, aimed at reducing the likelihood of future hospitalizations.
Evaluating the Effectiveness of Depression Treatment
Thankfully, effective treatments for depression exist. Psychotherapy, medication, or a combination of both have demonstrated positive outcomes in managing clinical depression, particularly in the absence of suicidal ideation. However, the persistence of symptoms in a substantial portion of diagnosed individuals underscores the need for ongoing care, necessitating continuous psychotherapy or medication management.
Empowering patients to engage in open dialogues with healthcare providers is crucial in tailoring the most effective treatment plan. While medication prescribed by primary care physicians remains a common approach, some cases may require specialized intervention from psychiatrists, psychologists, or other mental health professionals.
Statistics About Severe Depression
- Prevalence of Severe Depression in South Africa: Recent studies indicate that approximately 27% of the South African population has experienced severe depressive episodes, highlighting the significant impact of this mental health issue within the country.
- Suicide Rates Among South African Youth: South Africa has witnessed a concerning increase in suicide rates among youth aged 15 to 24, with recent data showing a 46% rise in suicide cases over the past decade, emphasizing the urgent need for effective intervention and support systems.
- Disparities in Access to Mental Health Services: Only 25% of South Africans suffering from severe depression have access to adequate mental health services, revealing significant disparities in access and highlighting the need for comprehensive initiatives to bridge the gap and provide equitable support for all individuals in need.
- Impact of Socioeconomic Factors on Depression: Research indicates that individuals from lower socioeconomic backgrounds in South Africa are 1.5 times more likely to experience severe depression, emphasizing the profound influence of socioeconomic factors on mental health outcomes within the population.
- Barriers to Mental Health Stigma Reduction: Despite increasing awareness, 37% of South Africans still perceive severe depression as a taboo subject, hindering open discussions and perpetuating stigmatization, underscoring the importance of targeted awareness campaigns and education initiatives to promote a more understanding and inclusive society.
Self-Assessment Tools for Depression Symptoms
Empower yourself with self-assessment tools designed to recognize the subtle signs of depression. Explore reliable resources that facilitate a deeper understanding of your emotional well-being and prompt timely intervention when needed.
Suicide Prevention Resources and Hotlines
Access a comprehensive list of suicide prevention resources and hotlines to ensure immediate support during moments of crisis. Gain insights into the crucial steps to take when encountering suicidal thoughts and learn about the vital services available to you or your loved ones.
Inpatient Care Facilities and Comprehensive Treatment Options
Discover the benefits of inpatient care facilities and their role in providing structured and intensive treatment for severe depression. Explore the comprehensive treatment options available, including psychotherapy, medication management, and expressive therapies, to facilitate a holistic healing journey.
Effective Communication Strategies with Healthcare Providers
Equip yourself with effective communication strategies to foster open and meaningful dialogues with healthcare providers. Learn how to articulate your emotions, concerns, and treatment preferences, ensuring a collaborative approach to managing your mental health and well-being.
Ongoing Support and Recovery Resources
Explore a range of ongoing support and recovery resources tailored to individuals managing depression. Discover the importance of continuous engagement with mental health professionals and access valuable resources to facilitate a sustainable recovery journey, promoting long-term well-being and resilience.
In exploring the complexities of severe depression, it becomes evident that timely intervention is crucial. Self-assessment tools aid in recognizing early symptoms, while access to suicide prevention resources remains pivotal during critical moments. Inpatient care facilities offer comprehensive treatment options, fostering a supportive environment for healing and coping strategies.
Effective communication with healthcare providers proves instrumental in tailoring personalized care, while ongoing support and recovery resources sustain long-term well-being. Despite challenges in access and stigma reduction, these initiatives serve as vital steps toward fostering a more empathetic and resilient society, echoing the essence of the initial call for open discourse on mental health.